COVID-19, Obesity, & Active Travel Behavior
Compact walkable environments with greenspace support physical activity and reduce the risk for depression and several obesity-related chronic diseases, including diabetes and heart disease. Recent evidence confirms that these chronic diseases increase the severity of COVID-19 infection and mortality risk. Conversely, denser transit supportive environments may increase risk of exposure to COVID-19 suggesting the potential for contrasting chronic versus infectious disease impacts of community design.
A handful of recent studies have examined links between density and COVID-19 mortality rates reporting conflicting results. Population density has been used as a surrogate of urban form to capture the degree of walkability and public transit versus private vehicle travel demand.
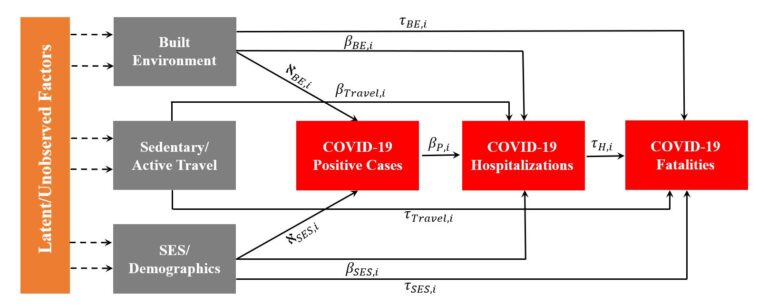
The current study employs a broader range of built environment features (density, design, and destination accessibility) and assesses how chronic disease mediates the relationship between built and natural environment and COVID-19 mortality. Negative and significant relationships are observed between built and natural environment features and COVID-19 mortality when accounting for the mediating effect of chronic disease. Findings underscore the importance of chronic disease when assessing relationships between COVID-19 mortality and community design. Based on a rigorous simulation-assisted random parameter path analysis framework, we further find that the relationships between COVID-19 mortality, obesity, and key correlates exhibit significant heterogeneity. Ignoring this heterogeneity in highly aggregate spatial data can lead to incorrect conclusions with regards to the relationship between built environment and COVID-19 transmission. Results presented here suggest that creating walkable environments with greenspace is associated with reduced risk of chronic disease and/or COVID-19 infection and mortality.

Most of the existing literature concerning the links between built environment and COVID-19 outcomes is based on aggregate spatial data averaged across entire cities or counties. In a separate study, we examined neighborhood level results linking census tract-level built environment and active/sedentary travel measures with COVID-19 hospitalization and mortality rates in King County Washington. Substantial variations in COVID-19 outcomes and built environment features existed across neighborhoods.
Using rigorous simulation-assisted discrete outcome random parameter models, the results shed new lights on the direct and indirect connections between built environment, travel behavior, hospitalization, and mortality rates. More mixed land use and greater pedestrian-oriented street connectivity is correlated with lower COVID-19 hospitalization/fatality rates. Greater participation in sedentary travel correlates with higher COVID-19 hospitalization and mortality whereas the reverse is true for greater participation in active travel. COVID-19 hospitalizations strongly mediate the relationships between built environment, active travel, and COVID-19 survival. Ignoring unobserved heterogeneity even when higher resolution smaller area spatial data are harnessed leads to inaccurate conclusions.

Publications:
Lawrence D Frank*, Behram Wali* (* denotes co-first authors). Treating two pandemics for the price of one: Chronic and infectious disease impacts of the built and natural environment. Sustainable Cities and Society, 103089. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8196511/
Wali, B., & Frank, L. D. (2021). Neighborhood-level COVID-19 hospitalizations and mortality relationships with built environment, active and sedentary travel. Health & Place, 102659.
Major Contributors:
Lawrence Frank, Ph.D. Professor, Urban Studies & Planning, UC San Diego.
Acknowledgement:
We would like to acknowledge the support of Department of Urban
Studies and Planning at UC San Diego and US Environmental Protection
Agency’s Office of Research and Development and Smart Growth Office.